Ultrasound guided sclerotherapy improves the safety, accuracy and efficacy when injecting large varicose veins. The ultrasound accurately maps the veins to be injected and helps guide the needle tip to the targeted vein. The sclerosing agent is then injected into the vein by continuous monitoring and also helps the phlebologist control the direction of the injection. Ultrasound guided sclerotherapy should only be performed by a phlebologist who has undergone specialized training, and is experienced in the procedure. We use micro foamed detergent type sclerosants for the procedure, such as Asclera. UGS makes it possible to easily treat the large trunk veins that are left after an endovenous laser ablation. It is also very useful to treat the large complex varices that can develop after vein stripping. Varicose vein disease is ongoing and even after an endovenous ablation procedure, patients sooner or later will probably develop collateral veins UGS makes it possible to easily treat these reoccurrences, before they become more of a problem, like phlebitis, ulcers, or dermatitis. We like to see all of our patients yearly after they have been treated for chronic venous insufficiency. UGS makes it easy to treat a small varicose vein if any have developed.
Click on any Category Below to Learn More
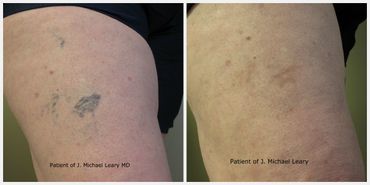
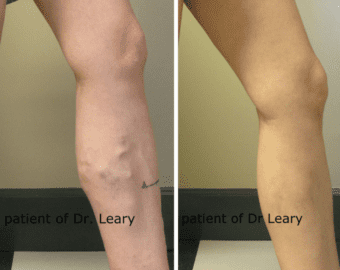
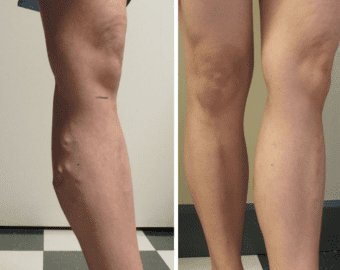
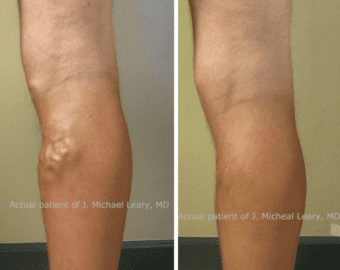
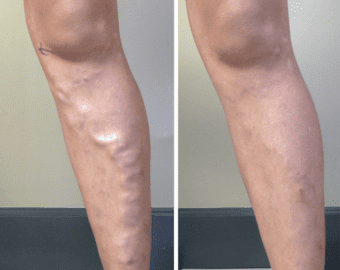
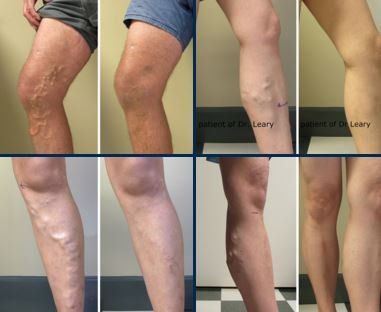
Expert Varicose Vein Removal For Beautiful Legs
Why Choose California Vein Specialists?
- Less Invasive Vein Procedures
- Same Day Ultra Sound in Our Office
- Highly Experienced, Knowledgeable Medical And Administrative Staff
- Personalized Treatment Plans
- Expertly Diagnoses And Skillfully Performs the Correct Treatment To Heal The Effects Of Venous Disease
- State-Of-The-Art Treatments With Minimally Invasive Medical Technology
- Excellent Follow-Up Care
- High-Quality Patient Care
Call us today for a vein screening exam at (949) 515-9377.
ENDOVENOUS LASER ABLATION
Endovenous Laser Ablation (EVLA) is a minimally invasive, more desirable alternative for the treatment of painful, unsightly varicose veins. With a 98% effective rate, varicose veins can be removed in the office and the procedure allows patients to return to normal activity immediately.
Advantages of Endovenous Laser Ablation
- Higher success rate
- Safer - Less risk of complication
- Easy and quick procedure – much improved due to latest technology
- Local anesthetic only – no general anesthesia
- You can drive yourself to the procedure and home from the procedure
- In-office procedure – no surgery center
- Less bruising
- Very comfortable procedure – Minimal pain
- Minimal post-procedure discomfort
- Return to normal activity immediately
“This is not the procedure my grandmother had! Had I known it was going to be this easy, I would have done it sooner” – Elizabeth S. Actual patient
While ligation and stripping was once considered the primary treatment for varicose veins, it has quickly become outdated and unnecessarily invasive. Ligation and stripping was performed under general anesthesia and required up to two weeks of recovery time before patients could return to work. Many patients also experienced pain and discomfort during and after the procedure, as it involves pulling the damaged veins out through several incisions in the leg. Some vein centers are still performing vein stripping. If you have been told you need vein stripping please get a second opinion.
New technology has allowed doctors to develop less invasive alternatives such as EVLA. EVLA uses laser energy to heat damaged veins and seal them shut. This is done through a tiny puncture in the leg that does not even require suturing, but still offers patients permanent, effective removal of damaged veins. EVLA is ideal for nearly any patient with large, painful varicose veins. Your doctor will perform an ultrasound exam in order to determine if this procedure is right for you. EVLA can be performed for medical or cosmetic purposes.
Recovery and Results
After the EVLA procedure, patients will be able to return home and to normal activities right away. Most patients return to work the very next day, although exercise and strenuous activity should be avoided for a few days. There is no stitching or suturing needed after this procedure. The puncture is small enough to heal on its own and leaves virtually no scarring.
EVLA provides permanent removal of varicose veins through a minimally invasive procedure with no downtime. In order to maintain the results of this procedure and to prevent further damage from occurring, patients are encouraged to lose weight, engage in a healthy and active life, and have an ultrasound on your veins yearly for early detection.
Risks
While EVLA is generally considered safe, there are certain risks associated with any surgical procedure. Some of these risks include infection, bruising, bleeding, clotting, puncturing and thermal damage. These risks are considered rare and most patients undergo the procedure with no complications.
If you are interested in learning more about EVLA, please call our office to schedule a exam. (949) 515-9377. There is no reason for you to be living with painful, unsightly varicose veins any longer, and relief is now available through this safe, minimally invasive procedure.
sclerotherapy
Foam Sclerotherapy
Sclerotherapy has made a major evolution with the introduction of Microfoam. Traditional sclerotherapy causes damage to the lining of the vein, causing it to collapse and making the walls of the vein then stick together. The vein is then slowly reabsorbed and disappears. Foam Sclerotherapy works in the same way only it is much more efficient. Foam is made by adding air to a liquid sclerosant such as the detergent Asclera. The liquid and the air are agitated to produce a foam mixture. The foam is then injected directly into the vein. Foam is not diluted like the conventional sclerosant, so much less is needed and it remains in the vein for a longer period of time. Foam also works better because it pushes the blood out of the vein and makes a better contact with the vein walls. This enables us to treat much larger veins with liquid Sclerotherapy.
Another advantage to using foam is that it is very echogenic, making it very easy to see on ultrasound. We can track the entire vein that has been treated. We also track the travel of the foam in a particular vein and stop the flow by applying pressure with the ultrasound probe, then flow can then be redirected if necessary. The selective treatment of veins with foam is more complete than with surgical removal or microphlebectomy.
“This is not the procedure my grandmother had! Had I known it was going to be this easy, I would have done it sooner” – Elizabeth S. Actual patient
Sclerotherapy
Sclerotherapy, the gold standard of treatments, involves injecting veins with a safe solution that causes the body to absorb the vein without harming the rest of your body. The success of the treatments is dependent on many factors, including the solution used, the technique of the physician, the general health of the patient, and the anatomy of the particular vein. Tiny needles are used, and complications are extremely unusual. The treatment involves no significant limitations or downtime, and the patient may go immediately back to work following their appointment.
Cryo Sclerotherapy
Cryotherapy delivers cold air onto the skin as Sclerotherapy injections are administered, making sclerotherapy an almost pain-free process. Our cryotherapy machine delivers short bursts of super-cooled air to numb the skin. The cold temperature is extremely effective as a topical numbing agent and also helps in reducing inflammation. This results in a more comfortable procedure, faster results and faster healing time.
Ultrasound Guided Sclerotherapy
Sclerotherapy vs. Laser when treating spider veins
Many laser centers offer laser treatment for spider veins, unfortunately laser treatment are not very effective for spider veins. With laser treatments it is impossible to get to the feeding veins that are actually causing the spider veins. There may also be a risk of burning the skin with laser treatment for spider veins.
If you are fortunate to have success with laser, they usually return because the underlying cause was not addressed. Laser are seldom as effective as injections for this reason. Sclerotherapy when performed properly is still the gold standard for treatment of spider veins. Successful treatment requires expertise in the art of sclerotherapy, the correct diagnosis and the correct treatment plan for the type and size of vein to be treated. Even small spider veins can sometimes be caused by underlying large veins that are incompetent. All sources of reflux should be ruled out by duplex ultrasound before proceeding with sclerotherapy even on small spider veins and webs. If not high failure rates can be expected and complications such as matting, hyperpigmentation and early recurrence can be expected.
If your doctor offers only laser therapy, be prepared for mediocre results.
Complications of Sclerotherapy
Sclerotherapy is an extremely safe and effective procedure when performed properly. As with any medical procedures complications can occur. I will review the most common and rare complications.
VARICOSE VEIN TREATMENT
In order for Dr. Leary to determine the cause and appropriate treatment of varicose veins, he will use a non-invasive ultrasound, which will help assist in evaluating the veins that are not visible on the surface of the skin and help decide the best treatment plan for a patient with varicose veins.
What Causes Varicose Veins?
To understand the causes of varicose veins, it is essential to review the primary function of veins and their basic physiology.
Remember, the heart pumps blood to supply oxygen and other nutrients to the entire body, so the heart pumps blood from the heart to the body parts. The veins carry the used blood or deoxygenated blood back to the heart.
The blood that is pumped back to the heart flows in these veins that act like one-way valves that keep the blood flowing toward the heart. In the legs, the calf muscle or musculovenous pump ejects 60% of the blood every time the calf muscle contracts. The calf muscle is the primary mechanism that returns blood from the legs back to the heart.
The veins returning blood from the legs have the toughest job of all the veins in the body because of the high pressure created by standing and the distance the blood has to be returned, and because of the force of gravity. This makes the leg veins the primary location of varicose veins and spider veins.
Without the correct blood flow, the blood reverses its flow and causes the valves to close improperly. When a valve fails to close correctly, it can cause a vein to swell, become painful, and bulging varicose veins. Increased pressure to the vein can cause a person’s legs or ankles to swell and to have severe pain and aching.
Heredity has a strong association with your chances of developing venous disease. If both parents have venous disease, you will have about a ninety percent chance to have the same. If you are female and have one parent with venous disease, you have about a sixty percent chance of developing varicose veins.
If you are male with one parent affected, your chances are about twenty-five percent. So women have more venous disease than men, but men that are affected normally have more serious complications such as ulcers.
What Are the Best Treatments for Varicose Veins?
We offer many different varicose vein treatments at our practice that can be used depending on your unique needs. These procedures are extremely safe and effective procedures. There are risks, as no procedure is risk-free.
Every procedure is tailored to the particular needs of the patient. Some patients will be better candidates for laser, while some may be better candidates for radio frequency. Dr. Leary will discuss and recommend which of these options he feels is best for each individual patient.
Here is a list of our varicose vein treatments:
How Much Does It Cost to Have Varicose Veins Treated?
The price of your varicose vein treatment will depend on the kind of procedure you are having performed. Your cost could range anywhere from $500 and $1,500 based on your specific goals, conditions, procedure and the amount of needed correction.
During your consultation, we will be able to give you a very clear idea of what kind of financial and time investment you will need to make to have the treatment performed. In some cases where the need is considered medically necessary, the procedure may be covered by insurance.
What Kind of Recovery Can I Expect from Varicose Vein Treatment?
Most varicose vein treatments are minimally invasive and will not require an extensive amount of recovery or downtime. Usually, patients will need one to two weeks to recover, but some treatments may require between three and four if the condition is severe.
Regardless of what procedure you have performed, you can expect to experience minor pain, redness, swelling, discomfort or soreness at the treatment area. This is normal and can be easily managed by over-the-counter or prescription medication.
How Can I Prevent Varicose Veins?
Why Dr. Leary?
Dr. Leary has a wealth of experience, education and expertise on venous concerns. He and his practice use only cutting-edge technology and techniques to ensure his patients the highest quality care possible.
Board Certifications
- American Board of Venous & Lymphatic Medicine
- American Board of Emergency Medicine
Professional Memberships and Accreditations
- Member, American College of Phlebology
- Diplomate, American Board of Venous & Lymphatic Medicine
- Member, American Venous Forum
- Member, American Society of Laser Medicine and Surgery
- Member, American Board of Emergency Medicine
- Fellow, American Board of Emergency Medicine
Frequently Asked Questions
SPIDER VEIN TREATMENT
The gold standard for treating spider veins and smaller veins is sclerotherapy.
Board Certified
Professional Memberships and Accreditations
- Member, American College of Phlebology
- Diplomate, American Board of Venous & Lymphatic Medicine
- Member, American Venous Forum
- Member, American Society of Laser Medicine and Surgery
- Member, American Board of Emergency Medicine
- Fellow, American Board of Emergency Medicine
Who should do the treatments for spider veins?
Have your veins treated only at a practice that specializes in phlebology. The doctor or nurse should be board certified or specially trained in phlebology. You should not allow non-physician treatment unless the doctor is on the premises or the provider is a nurse practitioner with special training. Seek out a center where the practice is dedicated to the treatment of venous disease.
Dr. J. Michael Leary at California Vein Specialists is a specialist in venous disease. He is board certified in phlebology and emergency medicine. He has specialized exclusively in venous disease for over nine years. Dr. Leary is a recognized leader in endovenous procedures, training many physicians from all over the United States.
HAND VEIN TREATMENT
Utilizing the latest technology, California Vein Specialists is committed to providing comprehensive minimally invasive vein treatments for the full spectrum of venous disorders from painful varicose veins to cosmetic spider Sclerotherapy, the gold standard of treatments, involves injecting veins with a safe solution that causes the body to absorb the vein without harming the rest of your body.
The success of the treatments is dependent on many factors, including the solution used, the technique of the physician, the general health of the patient, and the anatomy of the particular vein. Tiny needles are used, and complications are extremely unusual.3
The treatment involves no significant limitations or downtime, and the patient may go immediately back to work following their appointment.
Hand Sclerotherapy
The first step is to get rid of these large, bulging hand veins. These veins are normal, and more of a cosmetic problem than a disease process like varicose veins. Fortunately, the hand has plenty of venous return, and does very well when the veins are removed. The hand veins respond very well to sclerotherapy, typically with about two sessions.
The next step in
hand rejuvenation is volume replacement. The loss of fat in the hand makes the bones and tendons stick out and much more obvious, just like the veins. A very simple way of returning volume is to inject HA Filler,a common filler. HA Filler is highly malleable and when injected over the top of the hand it erases the bony look of the tendons and bones. The HA Filler injection is almost pain free because it is mixed with lidocaine, a local anesthetic. Once injected the HA Filler is massaged into a smooth natural appearing surface that replaces the fat that has been lost. HA Filler may last up to two years. Your hands will look and feel completely natural.
Board Certifications
- American Board of Venous & Lymphatic Medicine
- American Board of Emergency Medicine
Professional Memberships and Accreditations
- Member, American College of Phlebology
- Diplomate, American Board of Venous & Lymphatic Medicine
- Member, American Venous Forum
- Member, American Society of Laser Medicine and Surgery
- Member, American Board of Emergency Medicine
- Fellow, American Board of Emergency Medicine